Big Apple trip takes blood cancer research to next level
Blood cancer expert Dr Mark Williams and senior PhD student Katie Miari have just returned from New York where they took their research into drug resistance in Acute Myeloid Leukaemia (AML) patients to the next level.
The scientists, who are based in Glasgow Caledonian University (GCU) Department of Biological and Biomedical Sciences, said the US trip was a huge step on the road to finding new and effective treatments to help AML patients live longer.
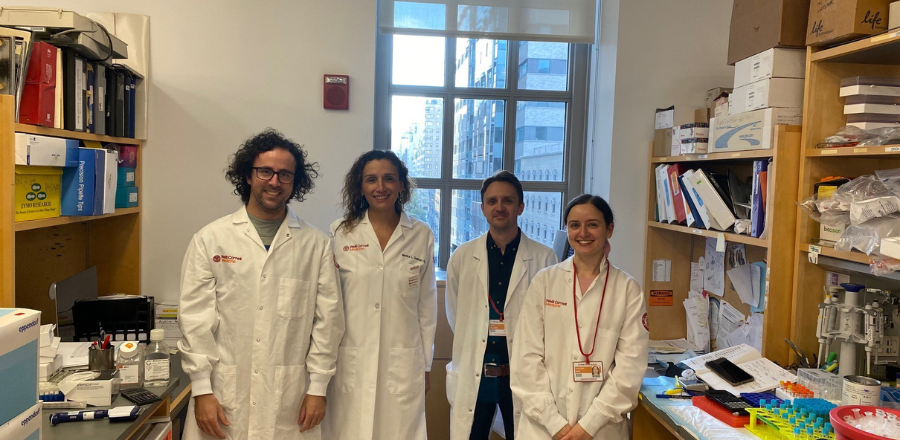
Dr Williams and Katie worked with world-leading AML expert Associate Professor of Pharmacology in Medicine Dr Monica Guzman and her team, in her labs at Weill Cornell Medicine Cornell University in New York for two months.
For the first time, Dr Williams and Katie were able to use leukemic cells and macrophages from AML patients that Dr Guzman’s lab has access to through a local Biobank.
This allowed them to confirm their own AML research findings, which show that macrophages protect leukemic cell lines from the killing effects of chemotherapy.
Macrophages are large white blood cells that are an integral part of the immune system. Their job is to locate and destroy disease causing organisms. However, in cancers such as breast and lung cancer there is a large body of evidence demonstrating that a particular subtype of macrophage, called a tumour-associated macrophage promotes cancer development and spread.
Dr Williams and Katie, who are key members in the School of Health and Life Sciences’ Research Centre for Health (ReaCH) Molecular Mechanisms of Long-term Conditions Research Group, were awarded funding to further their studies in the US.
Dr Williams was competitively awarded a Visiting Fellow Grant of £17,997 from the British Society for Haematology (BSH) to fund the eight-week research visit, while Katie received a prestigious European Haematology Association (EHA) Research Mobility Grant of £8,500.
Dr Williams has been working with Dr Guzman for over five years and he was the first scientist to import a key research technique from the US to the UK in 2018, with the long-term aim of increasing survival rates in patients diagnosed with AML.
Since then, he has been using the 3D model system to recreate how leukemic cells interact with macrophages which could help enhance the killing effects of chemotherapy and aid in the discovery of new targeted therapies for adults with AML.
Dr Williams said: “This is a very exciting time for our research into AML. Research from our blood cancer lab has shown that macrophages play a significant role in promoting cancer drug resistance, and through our research visit to Dr Guzman’s lab, we have now confirmed that this protective effect extends to clinically relevant patient samples, and not just AML cell lines.
“Given that cancer drug resistance is a major contributing factor towards treatment failure, disease reoccurrence and death in AML patients, it’s another huge step on the road to finding new and effective treatments to help AML patients live longer. Importantly, it could enable clinicians to predict the disease course of a patients, with the potential to target/modulate macrophages, as a way to personalise treatment for AML patients.”
Dr Williams has also recently been awarded a £105,591 Industrial Biotechnology Innovation Centre (IBiolC) collaborative training partnership (CTP) 4-year PhD studentship for his project entitled, ‘Generating a novel high-affinity multi-targeting therapeutic antibody for Multiple Myeloma’.
ReaCH aims to make a direct and significant contribution to Sustainable Development Goal 3 – good health and wellbeing – issued by the United Nations in 2015 as a blueprint for peace and prosperity across the planet.
Photo (left to right) shows Dr Leandro Martinez, Dr Monika Guzman, Dr Mark Williams and Katie Miari in the Guzman Lab in New York.
